Eagle Syndrome – What Every Voice Professional Should Know
Eagle Syndrome
I’ve been seeing more cases of Eagle Syndrome in my practice than the average statistics would suggest, and it’s made me reconsider the underlying factors that might be setting the stage for this complex condition.
What is Eagle Syndrome?
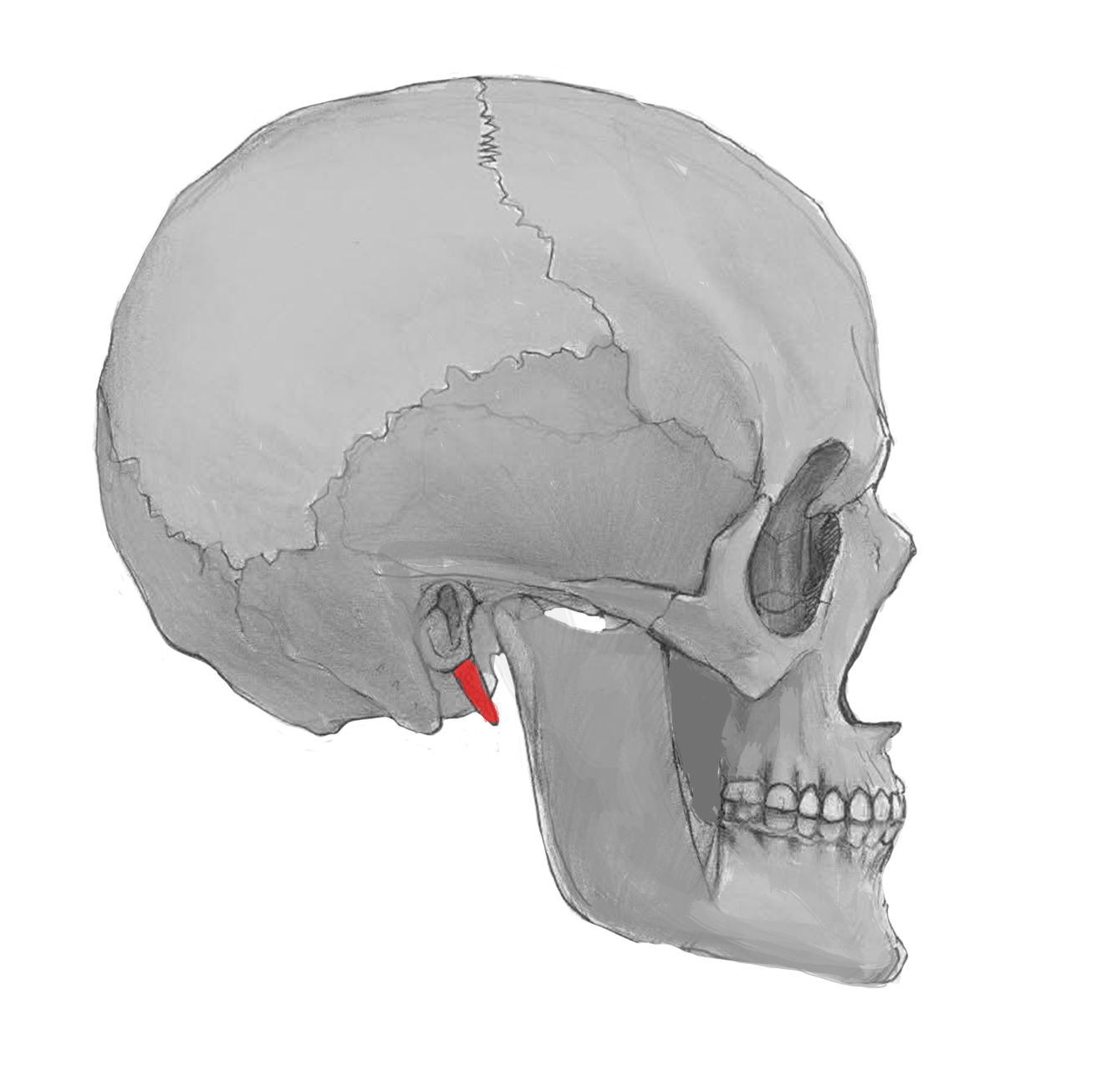
Eagle Syndrome involves an elongated styloid process or calcification of the stylohyoid ligament, leading to a range of symptoms like throat pain, ear discomfort, jaw issues, and even vascular symptoms if critical structures are compressed.
Why Does It Happen?
Though direct research is limited, I’ve noticed a pattern in many clients with Eagle Syndrome:
-
Early tonsil and adenoid issues
-
Chronic mouth breathing in childhood
-
Hypermobility or connective tissue laxity
The Childhood Connection – Why Early Airway Health Matters
Many children who undergo tonsillectomy or adenoidectomy do so because of chronic inflammation, frequent infections, or sleep-disordered breathing — all of which can often be traced back to mouth breathing and poor tongue function in early childhood.
Lately I have been thinking of ways it might connect:
-
Tongue Tie (Ankyloglossia) → Restricts tongue elevation, leading to mouth breathing
-
Mouth Breathing → Bypasses the nose’s natural filtration, humidification, and nitric oxide production
-
Chronic Inflammation → Enlarged tonsils and adenoids as the immune system reacts to unfiltered air
-
Postural Adaptations → Forward head posture, altered neck tension, and strained hyoid mechanics
-
Styloid Overload → Over time, chronic strain may encourage bony growth as a stabilizing response (though this part is more theoretical)
Hypermobility – Adding Another Layer of Complexity
For clients with hypermobility, the problem can be even more pronounced:
-
Less connective tissue stability
-
Greater strain on the stylohyoid complex
-
Increased risk of compensatory bone growth as the body seeks stability where it lacks it
While direct evidence linking hypermobility and Eagle Syndrome is limited, it may be possible that less stable connective tissue might increase the mechanical demand on the stylohyoid complex, potentially contributing to bony adaptation over time.
The Importance of Proper Imaging
CBCT or MRI of the head and neck by a dental or medical professional can provide essential information regarding length and position of calcification as well as relative risk for Eagle space compression.
A special thank you to my brilliant friend and colleague, Dr. Connie Brewster (DDS), for her insight and guidance around imaging standards and considerations.
Additional imaging like CTV or venography may also be necessary to determine impact on vascular structures. These studies are typically ordered by a neurosurgeon or ENT with specialty training in this area.
Why I Always Mention Eagle Syndrome in My Classes
I mention Eagle Syndrome in almost every class I teach—whether to manual therapists or university students—because awareness is critical. This condition is often overlooked but can significantly impact vocal health, airway function, and quality of life.
I also caution voice teachers who include manual work in their studios without a manual therapy license. Providing hands-on care without the proper training or understanding of complex conditions like Eagle Syndrome can unintentionally cause harm.
What to Watch For
-
History of tongue tie or early tonsil issues
-
High, narrow palate (a sign of poor early tongue posture)
-
Chronic neck, jaw, or throat pain
-
Forward head posture or altered cervical mechanics
-
Recurring ear fullness or difficulty swallowing
Next Steps
If you or a client is experiencing these symptoms, here are some supportive approaches:
-
Specialized Manual Therapy – Work with a licensed practitioner to address fascial restrictions and improve cervical and hyoid mechanics
-
Grounding Techniques – The grounding drills we practice in Vocal Resilience can help stabilize the OA (occipito-atlantal) joint
-
Breathing and Tongue Function Training – Restore nasal airflow and tongue posture to reduce upper airway strain
-
Collaborate with Airway Experts – Consult with a dentist or airway specialist who understands body biomechanics
Further Evaluation
If symptoms persist, a referral to a maxillofacial surgeon for imaging can help confirm a diagnosis. See The Importance of Proper Imaging above.
Want to Learn More?
Here are a few helpful resources recommended by colleagues:
From Caring Medical:
From Dr. Jeffrey Middleton:
Let’s Connect
Do you have experience with Eagle Syndrome, or questions about how it might impact the voice? I’d love to hear from you.
Stay well,
Christine
P.S. Are you interested in hearing how the OA joint impacts the rest of the cranial bones? We dive into the specifics in cohort 5 - Integration in The Visceral Voice Vocal Resilience Academy. Next cohort begins September 3rd.
TVV Insider
Join 1K+ readers of TVV Insider for leading edge insights on vocal technique, hyper-mobility, movement, biomechanics, coordination, strength, and mindset.

Responses